show/hide words to know
COVID-19 vaccines

In 2020, the race to make a vaccine against SARS-CoV-2, the virus that causes COVID-19, was a top priority for scientists. With so many types of vaccines, it's sometimes hard to understand how each one works. Let’s take a look at two main types: mRNA and viral vector vaccines.
The news was reporting these as new types of vaccines. But, it is important to know that both types of vaccines have been researched for decades to protect against many types of viruses, like Zika and Ebola. Current mRNA vaccines and viral vector vaccines that help protect against COVID-19 both contain genetic material that carries instructions to our cells. These instructions teach our cells to make a protein. The protein trains the immune system to fight against the virus that causes COVID-19. However; both types of vaccines differ in their ingredients, the type of genetic material used, and the way they deliver them.
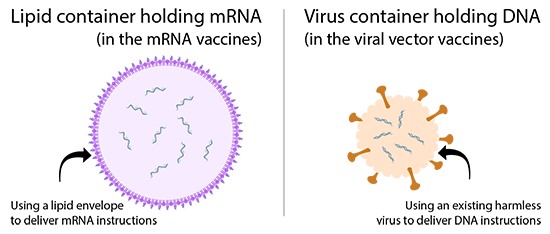
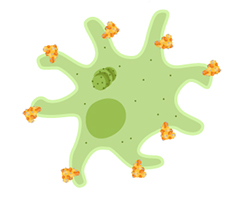
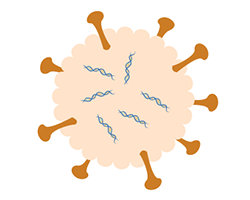
mRNA vaccines and viral vector vaccines both deliver genetic material to our cells so they can make proteins, but they do it in different ways. On the left, you see the delivery system used in mRNA vaccines - a small bubble or "nanoparticle" made of lipids (like oils) holding mRNA. On the right, you see the delivery system used in viral vector vaccines - a virus that is harmless to humans, that carries a piece of DNA from a different virus (the one we are trying to protect against). Click for more detail.
mRNA vaccines
Some of the first vaccines approved for public use against COVID-19 were mRNA vaccines. The mRNA vaccines from Pfizer-BioNtech and Moderna both give close to 95% defense against symptoms from SARS-CoV-2. Both vaccines need two doses at least 21 days apart (Pfizer-BioNtech) or 28 days apart (Moderna). In healthy recipients, both vaccines give close to 100% protection from severe COVID-19.
When thinking about “effectiveness” of the vaccine against COVID symptoms versus severe disease, what exactly does that mean? Effectiveness of the vaccines against COVID-19 "symptoms" refers to any symptoms experienced, even if they were very mild. Effectiveness against "severe COVID-19" or “severe disease” refers to more serious symptoms that could require medical attention. The most important thing to understand about all the approved vaccines is that they ALL offer ~100% protection from death caused by COVID-19, even if someone experiences severe symptoms. This highlights the importance of getting vaccinated, and not waiting for one particular type of vaccine, whether you get an mRNA vaccine, or a viral vector vaccine. Whichever you might get, let's take a closer look at how they work.
How mRNA vaccines work
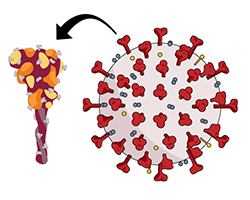
The viral protein we are using to teach our bodies how to fight off SARS-CoV-2 is found on the outside of the virus and is called the spike protein.
mRNA, or messenger ribonucleic acid, is normally in your cells and gives cells instructions to make proteins that cells need to function. COVID-19 mRNA vaccines contain mRNA that gives your cells instructions to make a protein called the "spike" protein of SARS-CoV-2. The spike protein is on the surface of SARS-CoV-2 and is the part of the virus that attaches to a cell’s surface to enter.
The spike protein on its own is harmless, and it cannot give you the virus. COVID-19 mRNA vaccines only make the spike protein of the virus and do not carry any live virus, which means someone cannot get COVID-19 from the vaccine. The mRNA itself is inside small capsules made of fats called “lipid nanoparticles.” These are taken up by your immune cells after you are vaccinated.
Once in the immune cell, the lipid capsules release the mRNA into the cytoplasm of the cell. The cell reads the mRNA's instructions and makes the SARS-CoV-2 spike protein. Next, your cell displays parts of this spike protein on its surface. This way, other cells are aware of the protein, and your immune system can respond to it. The mRNA never enters your cell's nucleus, the area where DNA is stored. All of the mRNA and other ingredients of these vaccines only stay in the body temporarily and do not alter your DNA.
After some of your immune cells have instructions for how to make the spike protein, they make it and move it to the surface of the cell. There, other cells can learn about the spike and how to launch an attack against it.
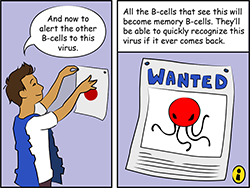
During an immune response to the spike protein, your body makes antibodies that attach to the protein. The immune cells that make those antibodies are replicated to make more until enough antibodies can be made to fight the virus. Other immune cells are recruited to find and kill the proteins marked with antibodies. The fight against the spike proteins in the vaccine is a way that your body learns how to beat the spike.
As a part of this process, your body will also make memory immune cells from the cells that were able to fight the protein. These cells should be able to recognize the spike proteins in the future, and make antibodies to the full virus, or kill infected cells, if the virus ever gets into the body. This process is much faster and more successful when your immune system has learned about the spike protein from a vaccine.
Long-term learning with vaccines
If SARS-CoV-2 enters the body after someone is fully vaccinated, antibodies made to fight the spike protein will quickly attach to the virus and act like little red flags. They will alert other immune cells to clear the virus. When attached to the virus, they can also physically block it from entering and infecting cells. This provides protection from infection for those vaccinated against SARS-CoV-2. Because your body recognizes important parts of the virus, it can fight it off much faster than it would have before, giving the virus little chance to cause a bad infection.
Viral vector vaccines
The Johnson & Johnson vaccine uses an adenovirus to deliver SARS-CoV-2 genes to our cells. This image of an adenovirus was taken with an electron microscope. Image by GrahamColm via Wikimedia Commons.
Some other vaccines approved for use against SARS-CoV-2 are viral vector vaccines. Viral vectors are versions of a harmless virus that are used to deliver genetic material from another virus to our cells. You can think of it as wrapping a tiny bit of harmless genes from one virus we want to protect against in the covering of another virus that won’t hurt us. The genetic material from the virus we want to protect against (in this case, SARS-CoV-2) holds instructions to make specific proteins in a cell.
Oxford-AstraZeneca and Johnson & Johnson vaccines against COVID-19 use viral vectors. Oxford-AstraZeneca’s vaccine caused at least a 63% reduction in symptoms from SARS-CoV-2 and close to 100% protection against severe SARS-CoV-2 after two doses. Johnson & Johnson’s vaccine is a single shot and is at least 66% effective overall in preventing moderate to severe COVID-19. The Johnson & Johnson vaccine is at least 85% effective at preventing severe COVID-19 and 100% effective at preventing death from COVID-19.
How do viral vector vaccines work?
Viral vector COVID-19 vaccines use harmless viruses to introduce genes from SARS-CoV-2 to our cells. Our cells use these genes to make proteins.
In the case of COVID-19 viral vector vaccines, the genetic material also contains instructions that tell some of your immune cells to make the spike protein. However; its instructions are made up of DNA instead of RNA. Upon vaccination, the viral vector will enter a cell, as a normal virus would. The vector will bring the DNA that contains instructions to produce the spike protein into the nucleus of the cell. There, the cell will begin to make mRNA that moves to the outside of the nucleus and into the cytoplasm. From there the spike protein will be made based off of the mRNA that was produced. The cell then displays parts of the spike protein on its surface, where the immune system can recognize it as an invader and launch a response.
Like mRNA vaccines, viral vector vaccines do not contain live SARS-CoV-2. So, someone cannot get COVID-19 from getting the vaccine. Additionally, the DNA contained in the viral vectors has been modified. The vector can enter cells but the genes needed for the virus to replicate have been deleted from the DNA. This means the viral vectors are not able to replicate in a cell, so they cannot cause disease. The DNA in the vector does not affect our cells because it is cleared after the protein is produced. These vaccines are more stable than mRNA and for this reason, may be kept for longer periods at higher temperatures than mRNA vaccines. This means these vaccines could be distributed to poorer countries without the ability to freeze the vaccine for long periods of time.
What to expect after getting vaccinated
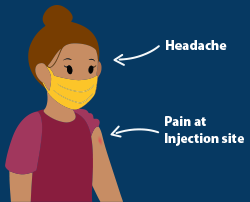
If people have side effects after being vaccinated, they are most likely to have pain at the injection site. Some may also experience a headache or fever, and feel tired. More serious side effects are very rare.
Vaccines go through careful safety testing before they are approved for public use in the United States. For COVID-19 vaccines, long-term safety data will continue to be collected. All of these vaccines may cause some cold-like symptoms. The most common side effects of the COVID-19 vaccines are pain at the site of injection, and possible headache, slight fever, and feeling tired.
It is important to know these symptoms are due to your immune system reacting to the vaccine and preparing to fight off the actual virus if the body ever comes in contact with it. For this reason, people should get the vaccine when they are eligible, to reduce the spread of COVID-19. Make sure not to take any unnecessary medications before or right after you get your vaccine. Some medications, like certain pain killers, may reduce the effectiveness of your immune system to launch a full attack during this training period.
Vaccines and variants
It is natural for viruses to mutate if they have spread from one person to another for some time. Since the Summer of 2020, we have seen this happening in SARS-CoV-2. Many people are worried that current COVID-19 vaccines may not protect against newly detected SARS-CoV-2 variants. So what does the science say about the variants?
Most variants have mutations in the virus’s spike protein. It is possible that some of these mutations may make the virus more contagious than the initial pandemic strain. This means that if a person is infected with a new variant, they could infect more people when sick than if they had the original pandemic strain. It is important to note that some SARS-CoV-2 mutations can affect vaccine effectiveness. However, these mutations are in only part of the spike protein, they don’t affect the entire spike.
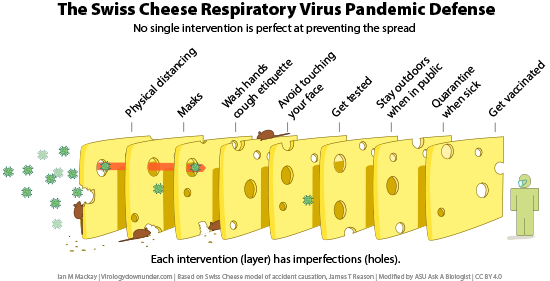
Current COVID-19 vaccines train the body to fight the entire spike protein. If someone is vaccinated and comes into contact with a variant, they should still have antibodies that work on the spike protein parts that were not mutated. So those antibodies should still help fight the mutated virus, even though in some cases they won’t be as effective. This does not mean people will not get sick at all from variants, but they will have better outcomes than had they not been vaccinated. These variants also provide a good reminder for many people that it is still important that we socially distance, use masks, and wash our hands, even after we've been vaccinated.
Vaccination with any of the available COVID-19 vaccines should still give some protection from the variants that have been discovered to date. For this reason, even if the vaccines are less effective against variants, some protection is better than no protection. It is important to get the COVID-19 vaccine to help stop the spread of all COVID-19 variants.
References
https://www.jnj.com/johnson-johnson-covid-19-vaccine-authorized-by-u-s-f...(link is external)
https://www.astrazeneca.com/media-centre/press-releases/2021/covid-19-va...(link is external)
https://www.cdc.gov/coronavirus/2019-ncov/more/science-and-research/scie...(link is external)
https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/(link is external)
View Citation

During the COVID-19 pandemic, many artists have painted street art as images of hope. Painting by Will Phillips.
Try our COVID simulator to experiment with how different safety measures can affect the spread of the virus that causes COVID-19.
Be Part of
Ask A Biologist
By volunteering, or simply sending us feedback on the site. Scientists, teachers, writers, illustrators, and translators are all important to the program. If you are interested in helping with the website we have a Volunteers page to get the process started.